In vitro fertilisation – or IVF – has allowed many couples with fertility issues to conceive. However, the relationships between different types of infertility and IVF outcomes are not yet fully understood. Male infertility can include non‐obstructive azoospermia, where sperm are not present in the ejaculate, and oligozoospermia, also known as a ‘low sperm count’. Men with these conditions can still have biological children through techniques such as surgical retrieval of sperm from the testes, in the case of azoospermia, and subsequent injection of an individual sperm into an egg cell. Identifying the effects of male infertility phenomena on subsequent IVF and pregnancy outcomes is important, so that couples can make informed decisions. Read More
Towards this aim, Dr Alexandros Grammatis of University of Athens and colleagues investigated the impact of sperm quality on IVF outcomes. Their study involved 1594 patients with different forms of male infertility.
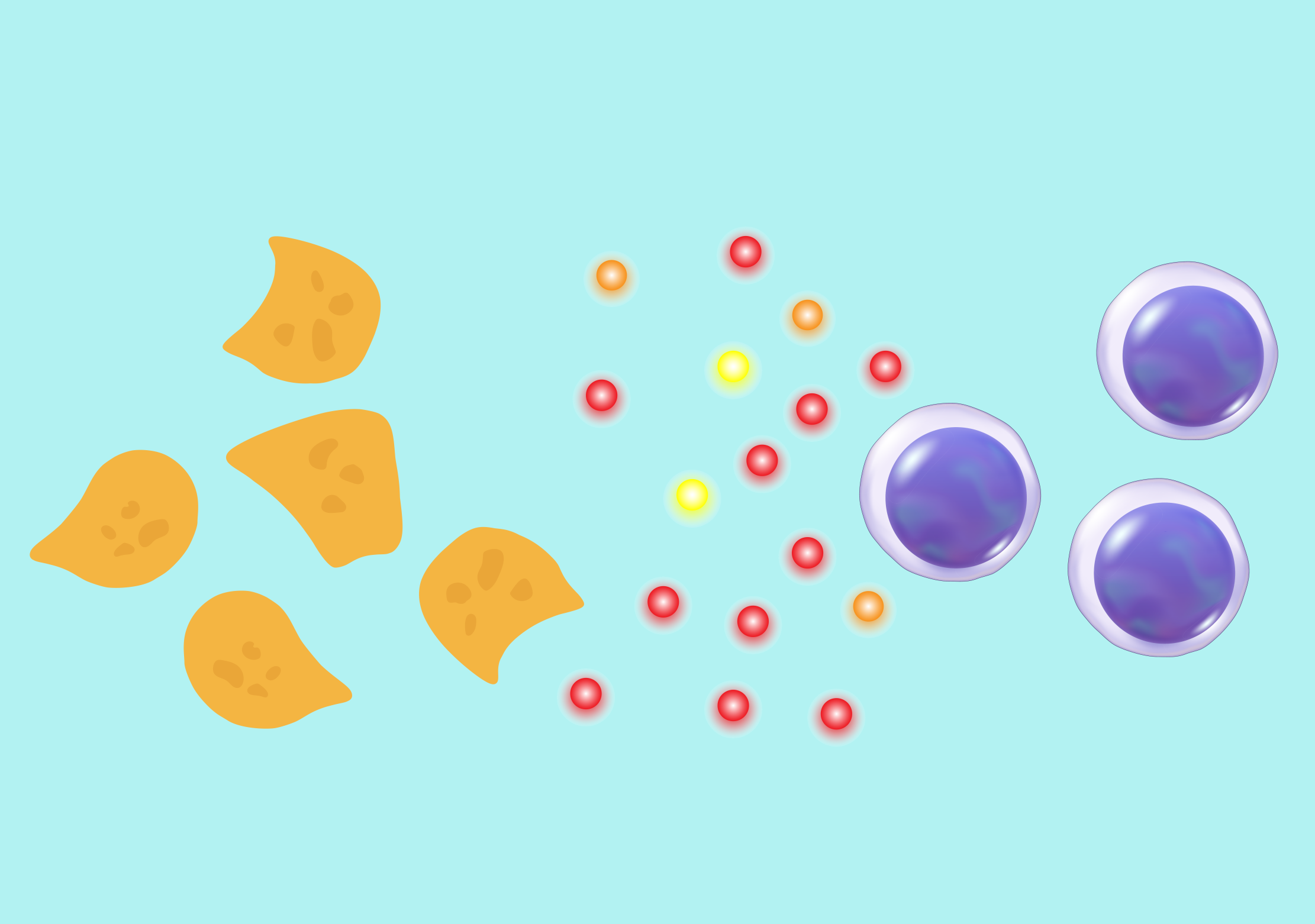
Sperm was collected from each patient, through surgical retrieval if necessary, and then injected into an egg to initiate fertilisation. Each egg was then transferred to the uterus of a female partner for implantation.
30% of the men had non‐obstructive azoospermia, where essentially no sperm are present in the semen. 28% had a severely low sperm count, with less than 5 million sperm cells per millilitre of semen, while 42% had a moderately low sperm count, with between 5 and 15 million cells per millilitre.
In the study, only IVF cycles using donor eggs were investigated. This is because donor eggs are typically taken from young women, and are considered high-quality. This allowed the researchers to isolate the effect of sperm quality.
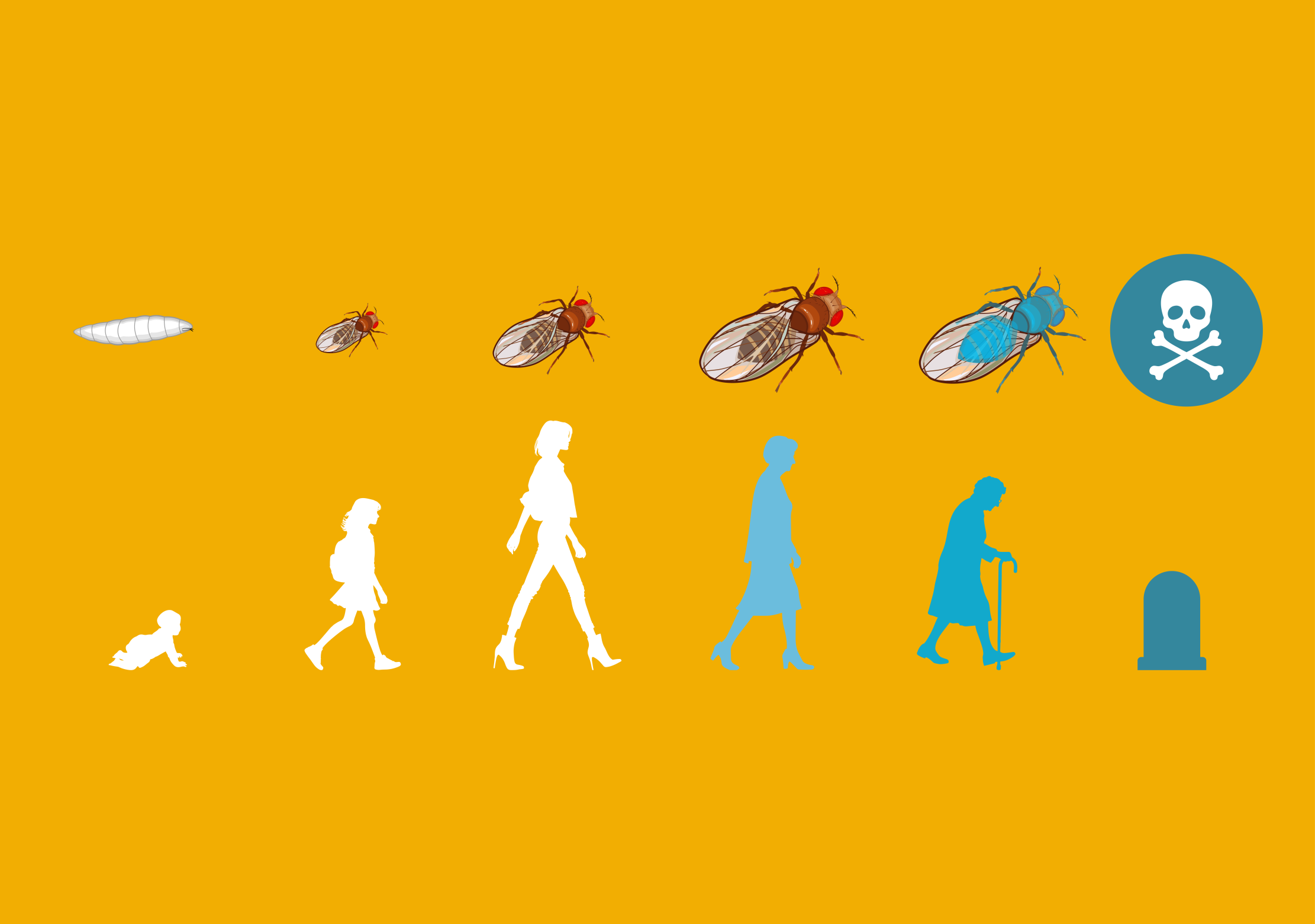
Following injection into a donor egg, the rate of successful fertilisation was low in the azoospermia group – at just 30%. This rate was 63% and 77% for the patients with severely low and moderately low sperm counts, respectively. The injected eggs in the azoospermia group also demonstrated a reduced chance of developing into an embryo with a typical number of chromosomes.
Following uterine implantation, the azoospermia group also demonstrated poorer outcomes. The miscarriage rate in this group was almost 12%, compared with 7% and under 3% in the patients with severely low and moderately low sperm counts, respectively.
The live birth rate per embryo transferred to the uterus was also reduced in the azoospermia group, at just 20%, compared with the low sperm count groups, which both had rates of over 30%. The risk of preterm labour was also higher in the azoospermia group, at 55%. This risk was 47% for those with a severely low sperm count and just 16% for those with a moderately low sperm count.
These results suggest that sperm quality not only affects fertilisation and implantation, but also pregnancy outcomes. Dr Grammatis’s study shows that sperm quality is closely linked with IVF and pregnancy outcomes. Couples with low or absent sperm levels who wish to conceive through IVF can now be better informed about their options and the most likely outcomes.