The liver plays a vital role in keeping us healthy, by controlling levels of sugars and fats in our blood, as well as clearing the blood of toxins. Chronic liver disease affects around 25% of the population and is reported to be the third largest cause of premature death in the UK. Liver disease can occur as the result of long-term consumption of alcohol or viral hepatitis, but the fastest growing cause is non-alcoholic fatty liver disease, associated with obesity and type 2 diabetes. Read More
Dr Matthew Hoare (of the University of Cambridge) and Dr Peter Campbell (of the Wellcome Sanger Institute) conducted a large-scale study to assess the genome changes in the liver caused by alcoholic- and non-alcoholic fatty liver disease. They sequenced a total of 1,590 whole genomes from 34 livers, including five from individuals with healthy livers, 10 from patients with alcohol-related liver disease, and 19 from patients with non-alcoholic fatty liver disease.
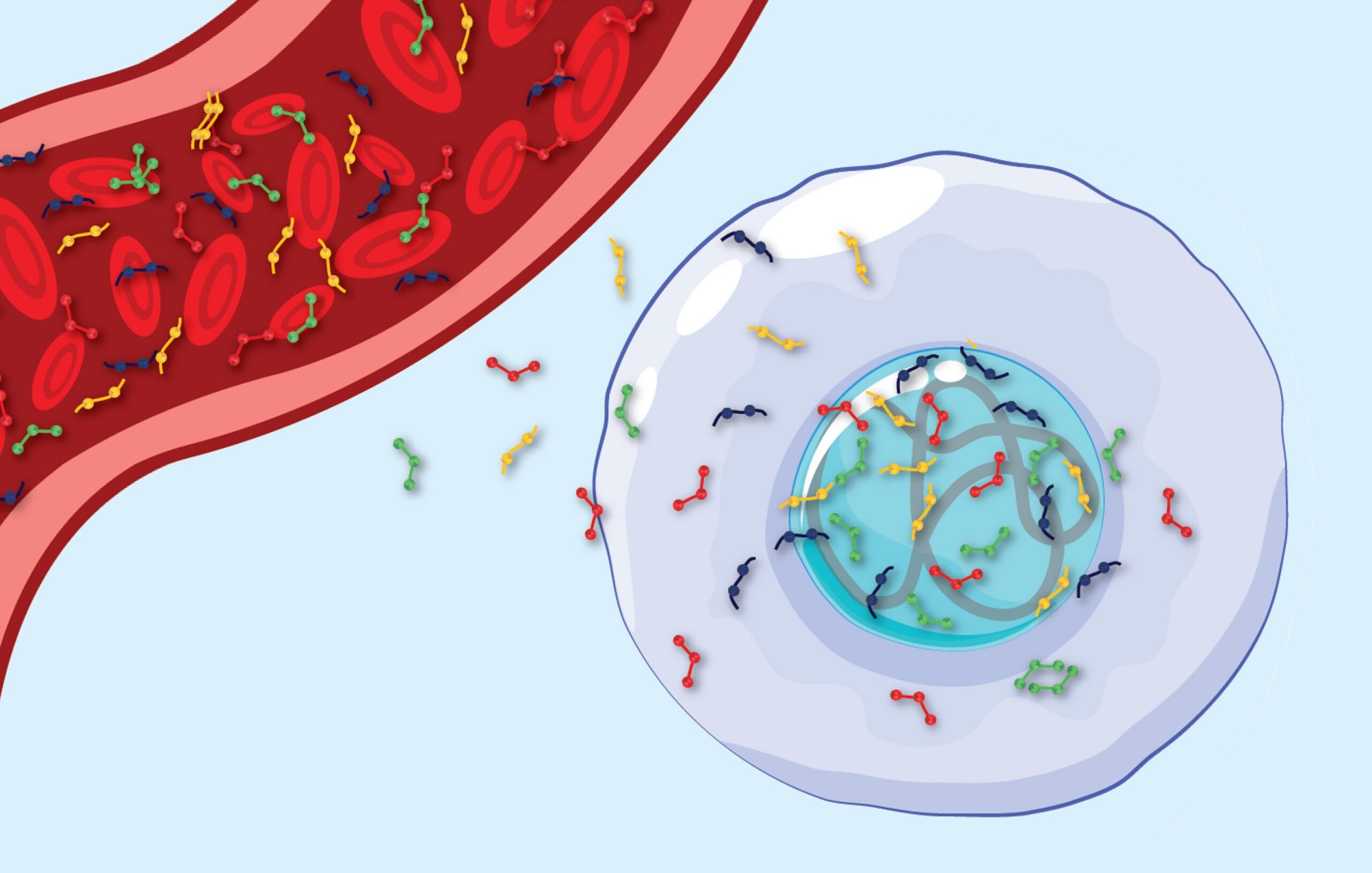
Dr Hoare, Dr Campbell and their team studied groups of hepatocytes – the primary cells found in the liver – to identify gene mutations under evolutionary selective pressure in chronic liver disease. They found hepatocytes had an increased DNA mutation rate. On average, the hepatocytes in diseased livers had around 1,250 more mutations than those in normal livers.
Several genes were mutated again and again in the unhealthy livers. One mutated gene in diseased livers, called ACVR2A, has been previously found to be mutated in some cases of primary liver cancer, known as hepatocellular carcinoma (HCC). This means that these mutations could be involved in liver cancer development.
The researchers also identified repeated mutations in three genes, all controlling major pathways involved in sugar or fat metabolism in the liver, that critically, had not been previously linked with liver disease or HCC.
These included mutatioms in CIDEB and GPAM, which both regulate the production and handling of fat within hepatocytes. However, the most intriguing finding was recurrent mutations in FOXO1, a major gene involved in the control of sugar metabolism and controlled by insulin. The mutations all affected the same location in DNA, leading to production of a mutant protein that had altered function – it’s movement was no longer controlled by insulin. This might mean that these mutations could worsen diabetes in people with liver disease.
Dr Hoare, Dr Campbell and their team were interested to discover if these mutations gave the hepatocytes carrying them a selective advantage – were they better able to survive and multiply than healthy cells? They found that groups of hepatocytes with mutations in FOXO1, CIDEB and ACVR2A were larger than their healthy neighbours, suggesting that these mutations give a selective advantage. The mutations help the hepatocytes to grow better than nearby hepatocytes without these mutations.
Future clinical studies will explore whether these mutations and genome changes are an indicator of the future risk of liver disease and cancer; If they do predict future health, whether they can be used in patients as biomarkers for disease progression and prognosis. Another exciting possibility will be to design drugs that harness or mimic the effect of these mutations to prevent the progression of liver disease and development of liver cancer.