Antimicrobial drugs treat infections by killing or slowing the growth of the responsible pathogens. However, antimicrobial resistance occurs when the bacteria develop defence mechanisms against the very drugs intended to kill them. Infections due to resistant bacteria can be extremely difficult and even impossible to treat, meaning that antimicrobial resistance presents a major threat to animal, environmental and human health. Read More
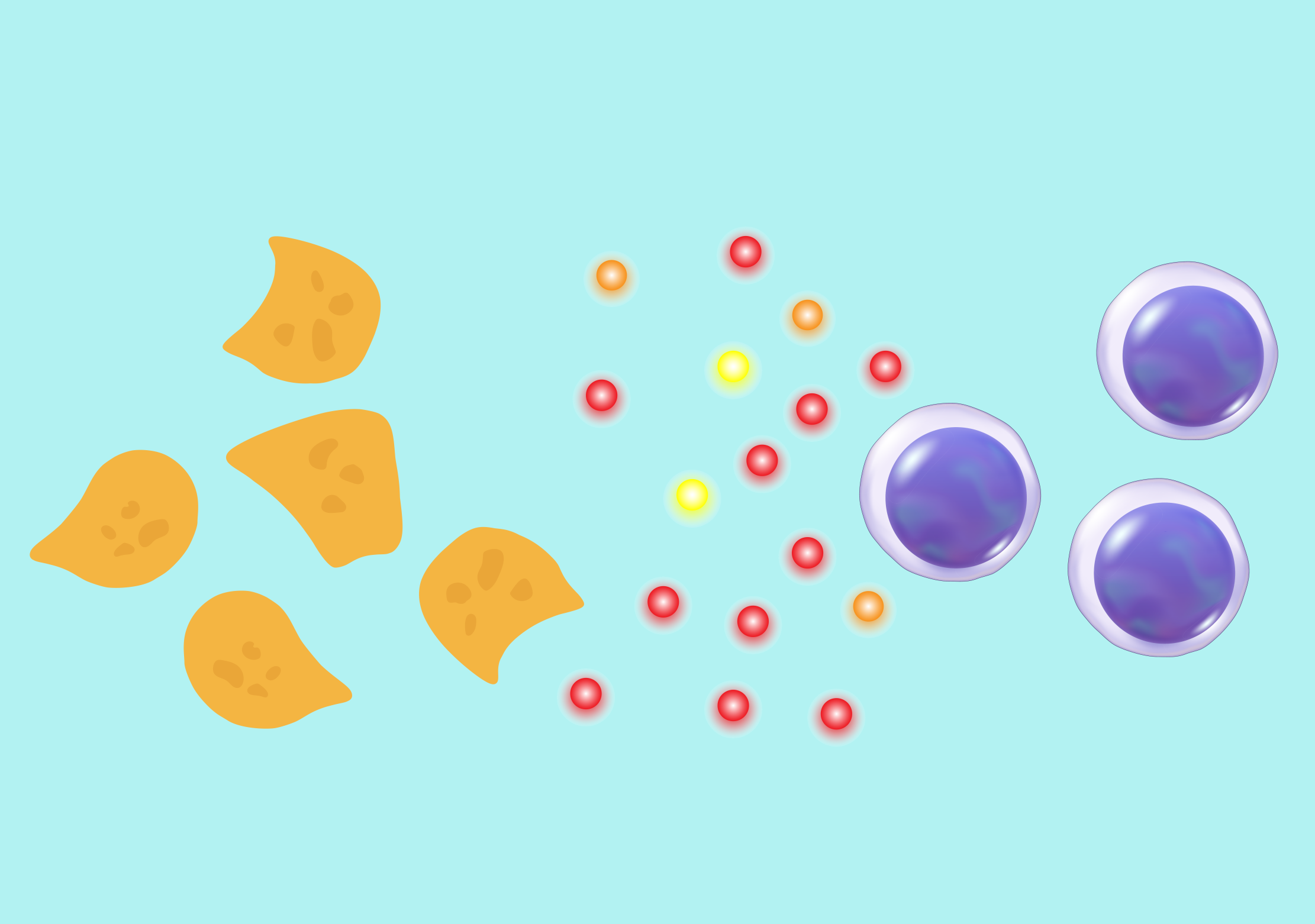
Antimicrobial resistance occurs naturally due to the presence of resistance genes in living organisms. Resistance genes can be acquired intrinsically through mutations or can be passed from bacteria to bacteria, via a process known as horizontal gene transfer. The genetic material involved in the transfer is a DNA molecule found within bacteria called a plasmid, which can carry just one or several antibiotic-resistance genes.
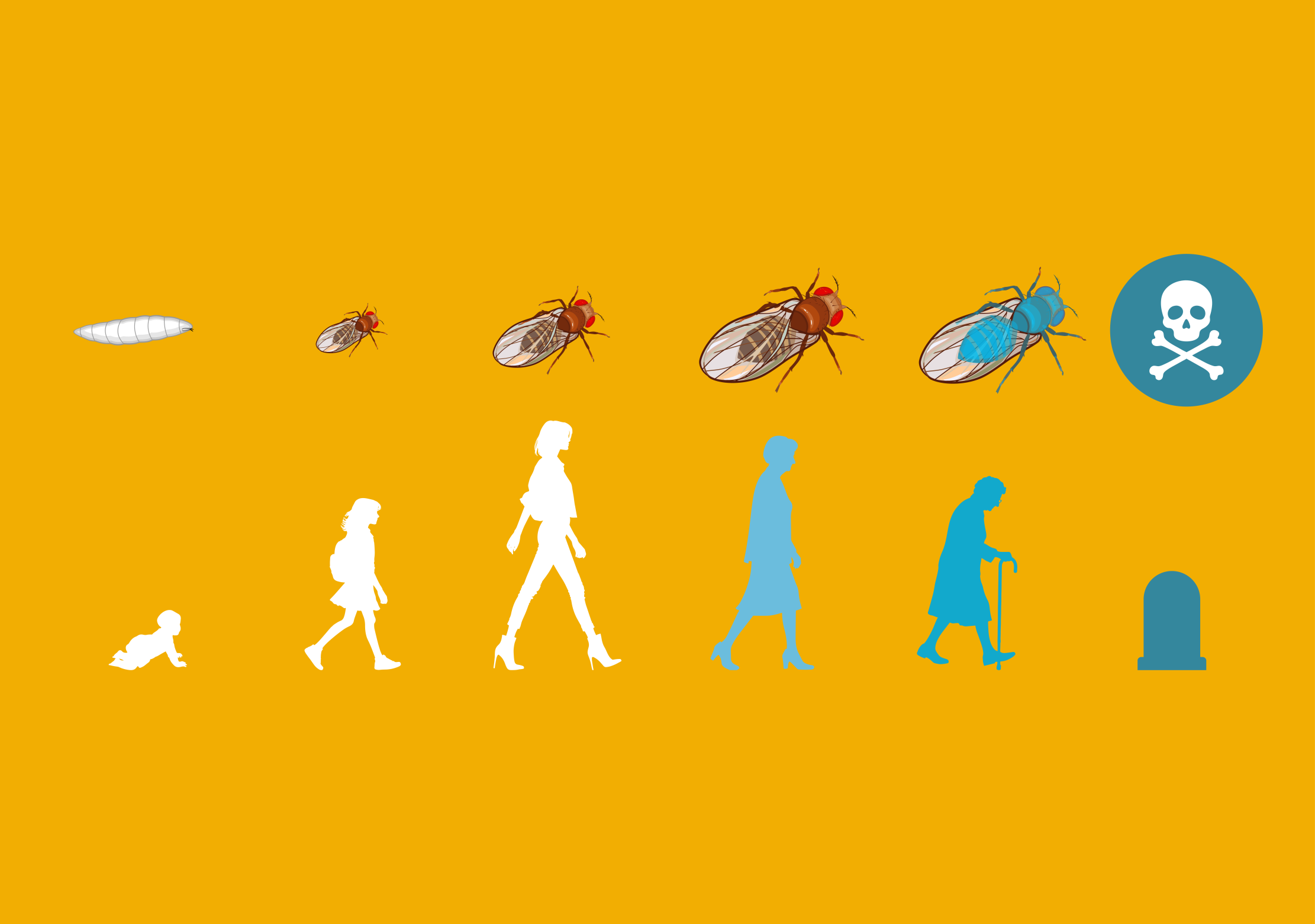
High risk clones are a relatively new concept described in the last decade. They are bacteria that enhance the spread of antibiotic-resistance genes. Through mutations and horizontal transfer, they acquired genetic characteristics that made them not only resistant to multiple antibiotics (thus intrinsically very difficult to treat), but also very well adapted to their environment and therefore very efficient in colonising different niches – that is, the functional role that each organism plays within an ecosystem. Consequently, high risk clones provide excellent vehicles for the plasmids involved in the transmission of antibiotic resistance genes.
For these reasons, they allow the rapid spread of resistance genes throughout a population of bacteria and among different species of bacteria, affecting humans, animals, food, plants, and the environment. It is crucial to detect and characterise high risk clones in animal populations to better manage the resultant difficulties, including the economic impacts.
Dr John Fairbrother at the Université de Montréal in Canada has worked with colleagues to propose a new definition of high-risk clones. Indeed, following a review of the literature, the researchers noted that important aspects of the previous definitions were not suitably adapted to the One Health approach. The One Health approach is a new collaborative, multidisciplinary and global method recommended by the WHO to apprehend public health issues, including human, animal and environmental health.
In their revised criteria, Dr Fairbrother and his colleagues proposed that a bacterial clone is high risk for antibiotic resistance spread if: (1) it is emergent, (2) carries multiple antibiotic resistance genes, (3) has a high capacity of spread, and finally, (4) is highly pathogenic.
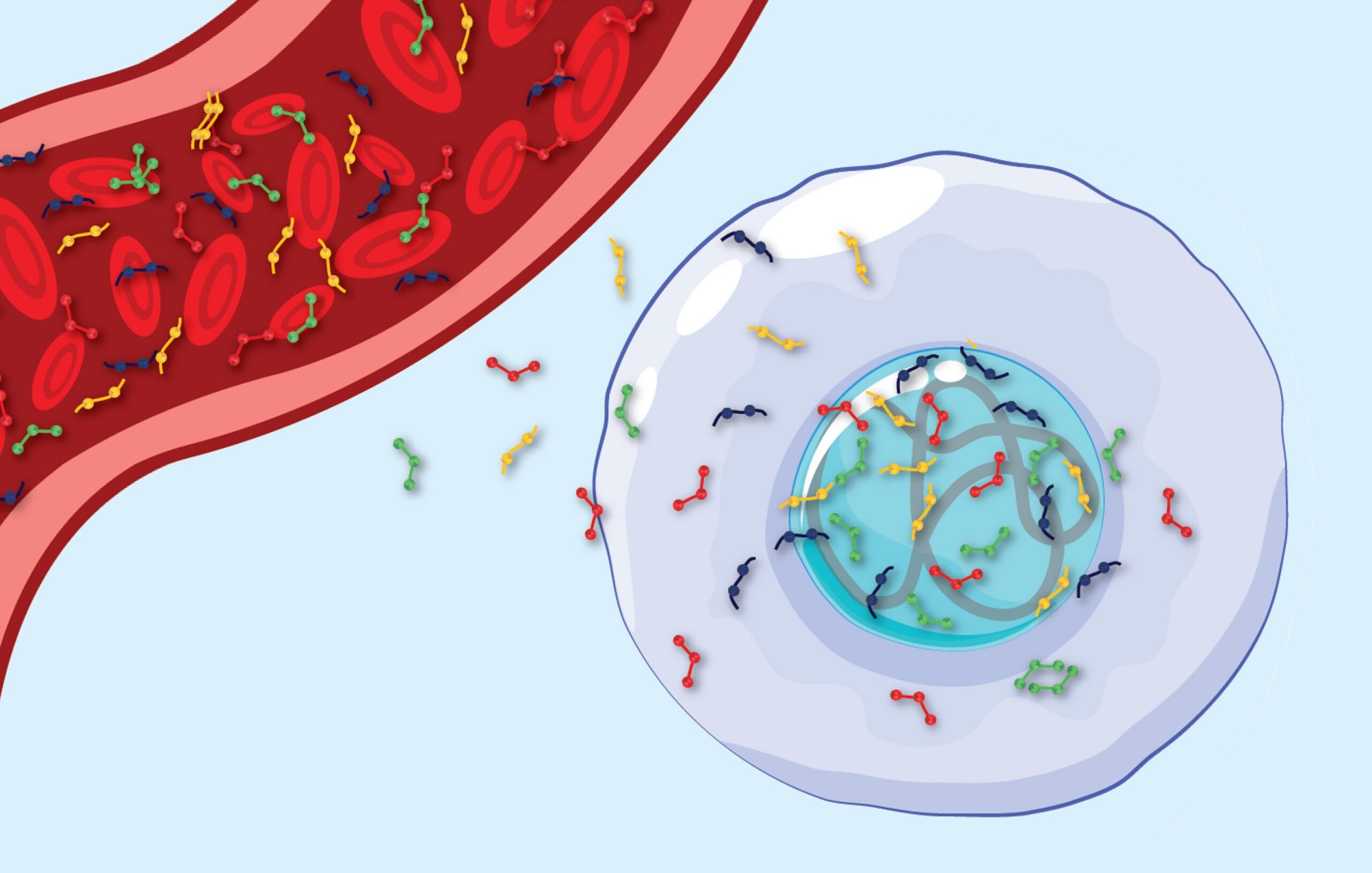
The researchers then applied their criteria to isolates of Enterotoxigenic E. coli (called ‘ETEC’) which emerged in 2013 in sick pigs in Quebec. The whole genomes (containing the entire genetic material) of 183 ETEC:F4 isolates collected between 1990 to 2018 were sequenced to determine their genetic code and the presence of virulence and resistance genes and plasmids was examined in 173 isolates. Then the isolates were compared to ETEC:F4 isolates collected in the USA.
Using their new criteria, the researchers demonstrated the presence of an ETEC:F4 high risk clone that emerged in 2013, in North America and threatened the pigs’ health. Consistent with their proposed criteria, it was found to be multidrug resistant, with a widespread distribution over the continent, that it was able to persist for several months on farms and finally, possesses a specific pathogenic and virulence genes profile.
The research team conclude that the ongoing surveillance of potential emerging clones is essential to increase our understanding of the factors that promote their occurrence and their spread, in order to inform effective combative strategies, such as vaccines.