Intrauterine adhesion is a common gynecological condition – one of the main diseases of the reproductive system. This uterine disorder is characterized by a partial or complete adhesion between the anterior and posterior walls of the uterine cavity and/or the cervical canal. It has a debilitating impact on the quality of life for women of childbearing age. Intrauterine adhesion can form when the lining of the uterus becomes damaged, leading to scarring or even obliteration of the uterine cavity. It can result from intrauterine infections and from operations such as dilatation and curettage after miscarriage or termination of pregnancy. Read More
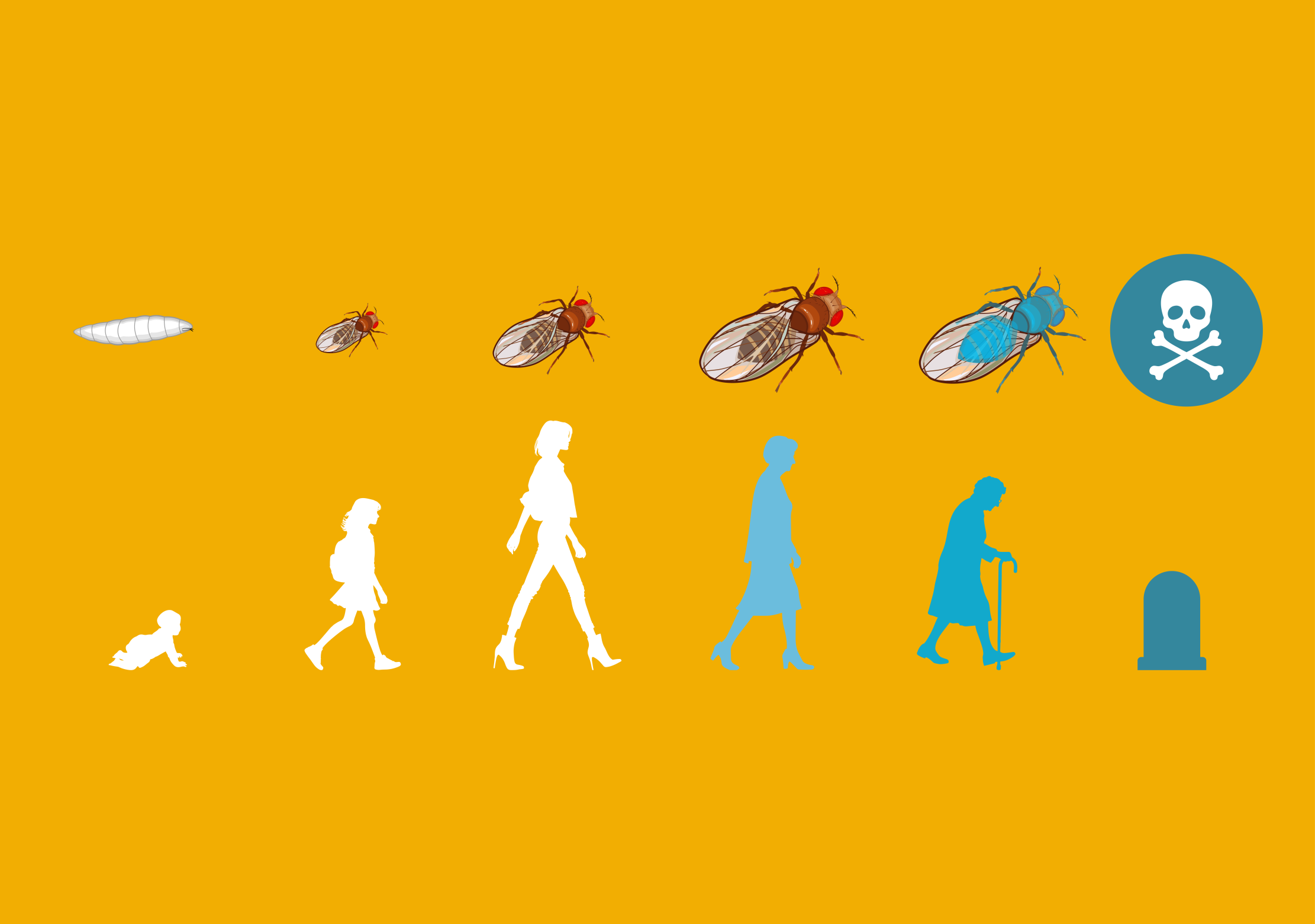
The consequences of intrauterine adhesion include menstrual disturbances, pelvic pain, infertility, miscarriage and complications during pregnancy and delivery. Early diagnosis, effective management, and prevention are crucial for addressing these challenges and improving reproductive outcomes. A large proportion of women who suffer from intrauterine adhesion wish to conceive again after treatment. However, the treatment of intrauterine adhesion continues to present significant challenges.
Dr. Angelo Hooker and his colleagues at Zaans Medical Center conducted a systematic review and explored the mechanism and interconnected processes leading to the formation of intrauterine adhesion, and the specific ways that the condition affects reproductive health. This knowledge enhances the understanding of adhesion formation and may lead to the development of new treatments, preventative strategies and diagnostic approaches.
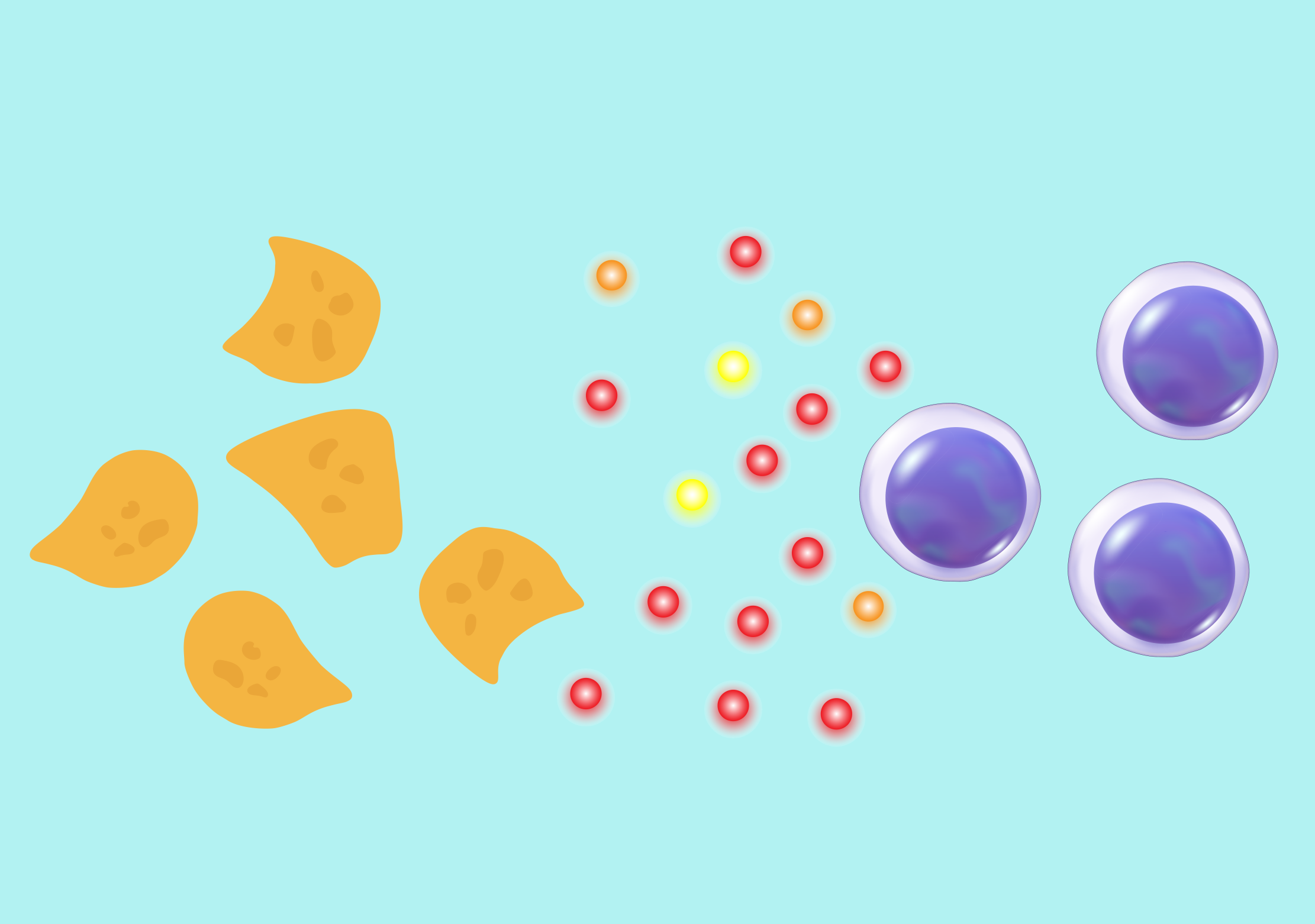
In their review, Hooker’s team analyzed 58 studies spanning decades of research, providing a comprehensive understanding of how intrauterine adhesion disrupts essential reproductive processes. The research shows that intrauterine adhesion interferes with sperm transport, prevents proper embryo implantation, and compromises placental development. These changes are exacerbated by reduced blood flow in the uterus, which results in a thinner, less receptive lining.
Hooker’s work also sheds light on severe complications that can arise during pregnancy and delivery. Women with intrauterine adhesion face significantly higher risks of conditions such as placenta accreta, where the placenta invades the uterine wall, leading to life-threatening bleeding during delivery.
Preterm birth, fetal growth restriction, and recurrent pregnancy loss are also more common in those affected. Remarkably, even after surgical interventions that aim to remove adhesions, the long-term effects of scarring often persist, impacting both fertility and pregnancy outcomes.
The review also emphasized how damage to the basal layer of the endometrium after different types of surgical interventions is critical in adhesion formation. To combat this, Hooker and his team highlighted the importance of preventive measures, such avoiding unnecessary surgery, and when needed, using minimally invasive surgical techniques and improving postoperative care to minimize trauma to the uterine lining.
In addition to prevention, Hooker’s team explored potential treatments. Globally, many anti-adhesion treatments have been used to improve reproductive outcomes and reduce the reoccurrence of the condition after surgery. However, an ideal treatment strategy is still lacking.
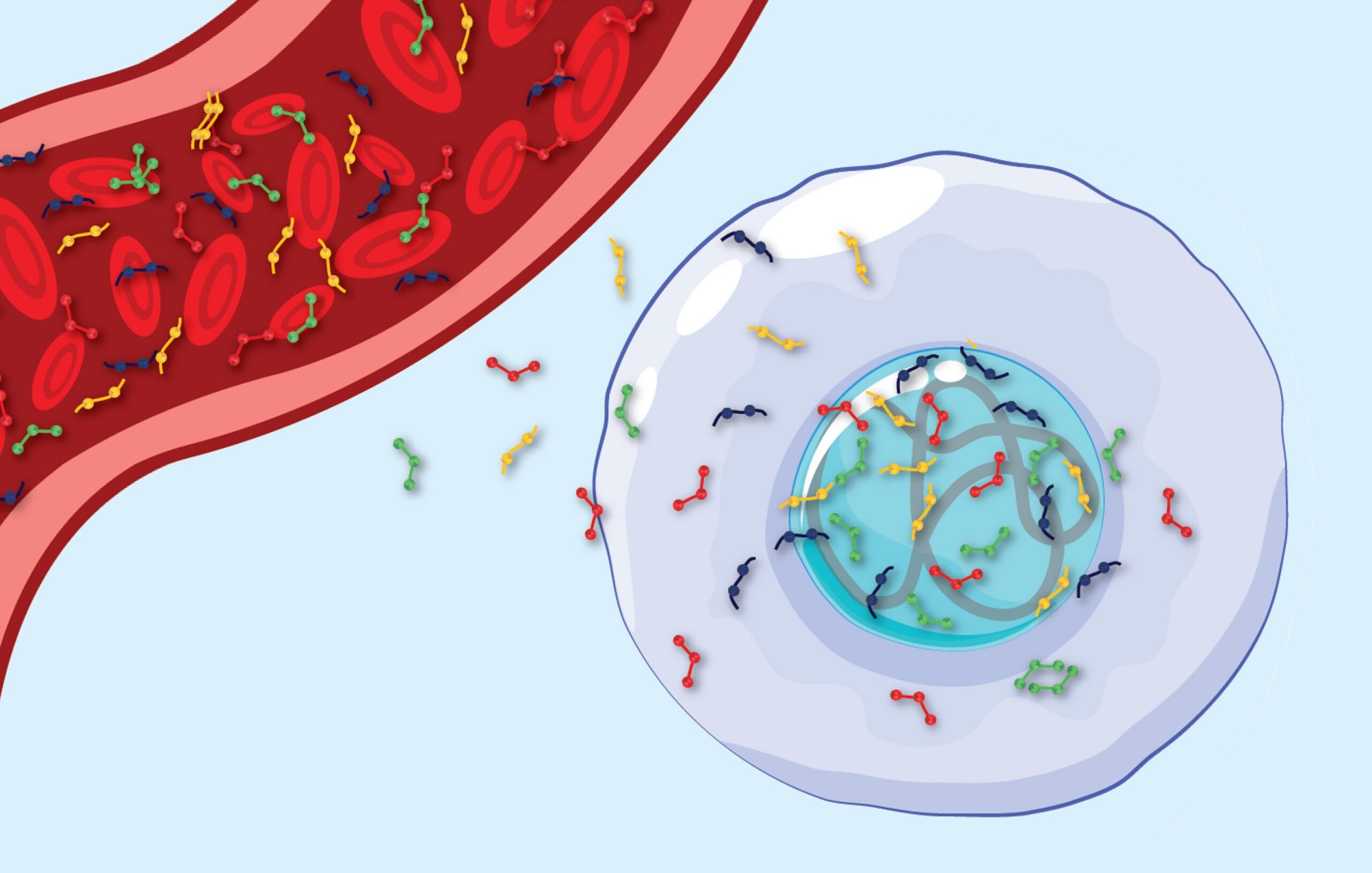
Regenerative therapies, such as stem cell treatments, are emerging as promising options to repair damaged uterine tissue and restore functionality. These innovative approaches could be transformative for women with intrauterine adhesion, offering new hope for recovery and improved health outcomes.
By investigating the underlying processes and mechanisms, and understanding the impact of intrauterine adhesion on reproductive health, Hooker and his colleagues have provided valuable insights into this complex condition.
While their review highlights the need for better understanding and awareness, it also outlines pathways for improving prevention, diagnosis, and treatment. For many individuals affected by this condition, this research offers hope for more effective care and a better quality of life.